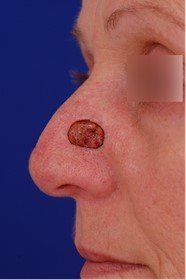
Tip of the Iceberg: A Skin Cancer Case Study
A 46-year-old woman who just moved to the US from Canada with her husband started noticing a rough patch on her nose that would not go away. She does not remember when or how it arose. There was never any pain or bleeding. She tried multiple skin cleansers, facial scrubs, and microdermabrasion without any lasting success.
Growing up, she had spent many summers at her family lake home. Prior to moving to the US, she and her husband camped often and enjoyed the outdoors in Canada. She was skeptical that she had a skin cancer — no one in her family had ever had one, and she thought living in Canada reduced her risk of ultraviolet exposure.
She was skeptical that she had a skin cancer — no one in her family had ever had one, and she thought living in Canada reduced her risk of ultraviolet exposure
When she finally saw a dermatologist, a biopsy was performed, and she was found to have a basal cell cancer (the most common form of skin cancer). The dermatologist correctly counseled her that basal cell cancers rarely, if ever, spread to other parts of the body, but they do continue to grow and may cause disfigurement. Also, now that she had one skin cancer, she was at greater risk than the general population of having future skin cancers.
To remove her cancer, she would need to undergo Mohs micrographic surgery, the best technique we currently have to reduce the risk of recurrence. She elected to have a plastic surgeon perform the repair. After the Mohs procedure, she came in to see me:
I decided to repair her nose in the office by moving some tissue from her cheek to fill the defect. In order to do so, wedges of tissue both above and below the defect site were to be removed. Noticed we designed the incisions to camouflage them as best we could around the nostril crease.
The patient healed well, but two months later she began to have new lesions show up on the right side of her nose. She underwent Mohs surgery again for another basal cell cancer removal and returned to my office after.
It seemed to me that something more was happening on the tip of her nose. To be safe, I decided to repair the area with a skin graft. Sure enough, two months later she came to my office distraught with this:
The patient had always disliked her nose and requested a rhinoplasty and repair at the same time. She wanted to remove the hump on her bridge and refine the tip of her nose. Unfortunately, the standard repair for this type of defect is a forehead flap. This is a two staged repair where skin from the forehead is bridged to the nose. Then, three weeks later, the bridge is removed and the forehead skin is left behind to fill the defect. The patient was adamantly against this, so we attempted a riskier flap where tissue from the nasal bridge is completely disconnected (except for two blood vessels on both sides) and moved downward. We performed this delicate operation as well as a rhinoplasty in the operating room. The intraoperative photos may be disturbing, but if you would like to see them, you may click here.
The patient did well, and six months later, she was cancer free and healing well:
This is a cautionary tale and a reminder that no one is safe from the accumulated effects of a lifetime of sun exposure. Please make sure you check yourself for any skin irregularity that persists for greater than 2 weeks and make regular visits to a dermatologist!