Nasal Airway Surgery
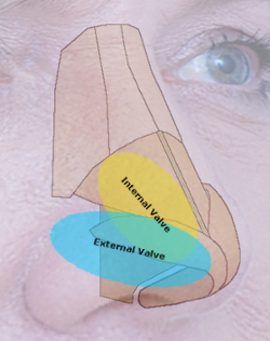
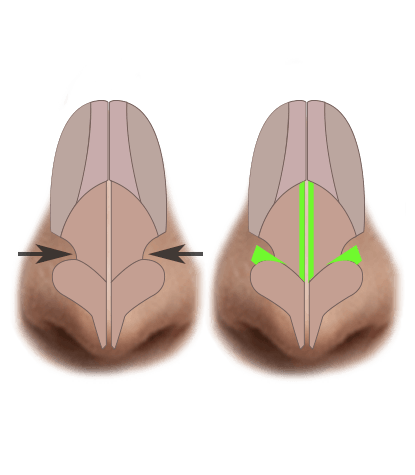
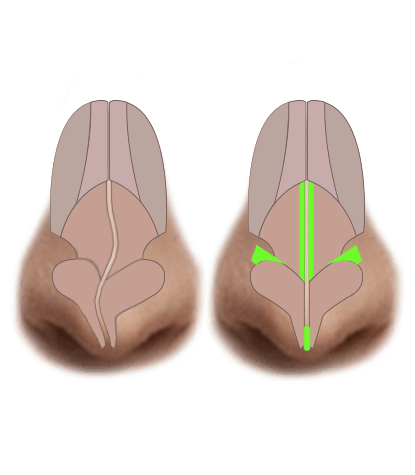
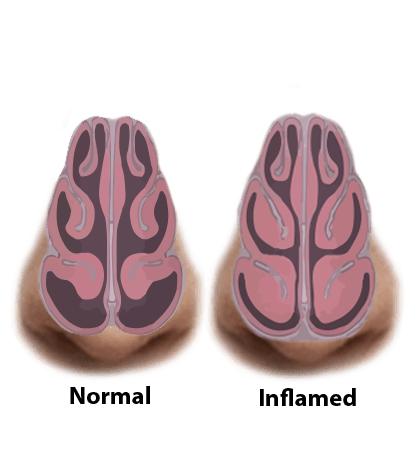
Those of us without problems breathing through our nose take it for granted. Those with nasal congestion and obstruction know they can have a debilitating effect. It can ruin our sleep, impair physical performance, and diminish our overall health. For this reason, procedures to correct these conditions are typically covered by health insurance. There are a wide variety of conditions that affect nasal breathing including a deviated nasal septum, hypertrophic turbinates, internal and external nasal valve collapse, and nasal septal perforations. We specialize in correcting these issues to help patients breathe better. A more functional airway can lead to reduced sinus symptoms, better use of CPAP devices for sleep apnea, and even reduced snoring.
"I was fortunate enough to get a recommendation to see Dr. Patel after having open rhinoplasty and a revision for a deviated septum from a surgeon in a different location. He was confident that he could make the changes I needed with a tip revision and also fix the scar that I was left with before. During the consultation, I told him to do whatever he thought I needed and that I totally trusted his judgement. I’m so glad I did that because my nose turned out PERFECTLY! 10 days later, my incision that Dr. Patel revised had already healed and it wasn’t apparent that I had surgery at all except my nose was straight and actually blends with the rest of my face verses looking out of place. I could not be happier!!!!!"